Biopolymer stents will make atherosclerotic cells healthy
30 October 2019 г.
The Krasnoyarsk scientists are carrying out long-term studies of natural polymers with a unique set of properties. These structural materials are biocompatible and biodegradable, which opens up almost unlimited prospects for practical applications, including regenerative medicine. Products from these materials are able to maintain the shape imposed by scientists, which implies that they can be used for creating various complex implants and bulk products for tissue engineering.
Biodegradable polymers are obtained using the microbiological biosynthesis, a process in which specific bacteria accumulate matter inside their cells. For the biosynthesis of polymers, bacteria have a special enzyme which combines individual organic molecules into long chains. These reserve macromolecules are synthesized by bacteria when grown in suboptimal conditions, for example, when they lack nutrients.
As part of the project supported by the Russian Science Foundation, the Krasnoyarsk scientists began developing individual coatings for vascular stents. They are used to eliminate angina pectoris in patients and after myocardial infarction. This task appeared due to a number of medical problems with traditional vascular stenting. When installing a stent made by filigree laser cutting of the thinnest, up to two millimeters in diameter, steel tubes, there is a risk of repeated narrowing of the vessel in the same place, due to the foreign body irritating the vessel.
In fact, the necessity for a stent to be in a heart does not last long, for about two to three weeks. During stenting, the atherosclerotic lipid plaque is destroyed - a growth that narrowed the vessel and caused discomfort and pain. The stent acts as a spacer, which prevents compression and ensures stable blood flow. The reaction is eliminated in two to three weeks, after which the spacer is no longer needed.
However, it is impossible to remove the “ingrown” stent since it has become a part of the vessel and prevents the formation of a “healthy” inner layer of cells. The metallic foreign body causes chronic inflammation and development of repeated, often rapid, atherosclerotic changes. The vessel in this place becomes less rigid than the healthy one, and the wall becomes more fragile, which can result in a rupture, i.e. vascular accident.
It is not surprising that in the world scientists are trying to develop temporary stents from degradable materials - polymers or metals. Magnesium and its alloys are used as biodegradable metals. The biocompatibility of such materials is low. In contrast, biopolymers of the Krasnoyarsk scientists are not rejected by living tissues. Moreover, changing the polymer structure during its biosynthesis, researchers can adjust the "lifetime" of the product in an organism, its flexibility and elasticity, as well as the surface topography.
When developing bioengineering structures implanted in a living tissue, one must take into account that their surface affects the activity of tissue cells. This is due to the transfer of mechanical force applied to the surface of a cell into biochemical reactions inside the cell. A cell in a tissue or organ is in the state of compression-tension balanced from different sides. On the one hand, neighboring cells and external components of the tissues — elements of the extracellular matrix — stretch it from outside. On the other hand, from the inside, forces arising due to the interaction of internal components of the cell with the membrane.
Changes in external physical parameters lead to the cell changing its shape, functional state, and even specialization. This means that by developing an external cell framework with certain parameters, scientists can make it change into the right direction. For example, in the case of atherosclerosis, we could prevent repeated atherosclerotic plaques, “forcing” the inner layer of vascular wall cells to form a rigid cell layer.
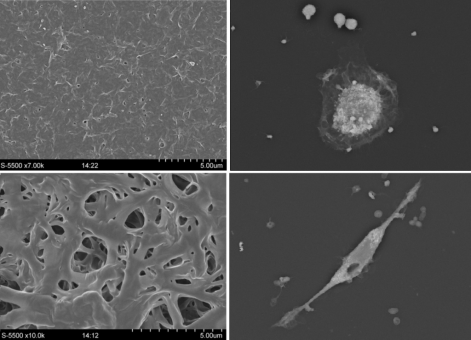
Currently, the Krasnoyarsk scientists are studying the mechanical and chemical interactions between biopolymers of different compositions and blood cells of patients with atherosclerotic plaques in the heart vessels. The blood samples for the study is provided by the Krasnoyarsk Cardiology Center, where it is taken from patients to be subjected to stenting. In the laboratory conditions, the cells from the blood of the patients begin to accumulate lipids due to their donors suffering from atherosclerosis, which means that their lipid metabolism is “shattered”. The task of the scientists is to study the nature of the interaction of cells with various materials, and, in the future, with the help of a biodegradable coating, to stop negative reactions.
“In the development of atherosclerosis, lifestyle, diet, and, unfortunately, heredity, are of great importance. If people who have this disease could see the way we see this problem, how their cells are filled with fat droplets and actually die, turning into motionless and “disabled” cells, they would readily follow the recommendations of their doctors. After all, the doctors’ advice is quite simple, which is not to eat fatty and salty food, and to move more, ”says Ekaterina Shishatskaya, head of the research, Doctor of Biological Sciences, head of the Department of Medical Biology at the Siberian Federal University, chief research associate at the Institute of Biophysics of the Krasnoyarsk Science Center SB RAS.
In addition to the visible accumulation of lipids - small dense droplets filling the cytoplasm, atherosclerotic cells, after contact with the biopolymer, strongly change their shape and production of molecules characteristic of the disease, such as prostaglandins and leukotrienes. The scientists found out that the cell response to polymer films of different compositions is different. In the future, this opens up possibilities for managing their condition.
“Our task is to bring the study to a stage where for a person suffering from atherosclerosis of a particular stage and having certain shifts in homeostasis, it will be possible to recommend the composition of the material to cover the biodegradable stent. The “ideal” material will allow the affected vessels of the heart to heal without a trace of the plaques which were once present. Subsequently, this material can be used to produce the entire stent, and even for more complex implants, such as fragments of blood vessels, valves and the whole heart, ”explains Ekaterina Shishatskaya.
Share:
