Golden killers of cancer cells
31 March 2021 г.
A team of Krasnoyarsk researchers has been working for several years on a project for the selective destruction of cancer cells by nanoparticles of gold and other metals.
With the help of special biological molecules, such particles are targeted to malignant cells, and then, these cells are destroyed through various physical impacts, including laser radiation.
For targeted delivery, aptamers, in other words, "guide molecules", are usually used. These are artificial single-stranded DNA or RNA sequences. Such delivery systems are called bioconjugates.
This is a joint work of scientists from the Federal Research Center "KSC SB RAS", L.V.Kirensky Institute of Physics, VF Voino-Yasenetsky Krasnoyarsk State Medical University and Siberian Federal University.
One of the first notable publications of Krasnoyarsk scientists in the world scientific periodicals, dealing with the results of such studies, appeared in September 2017 in the journal Molecular Therapy.
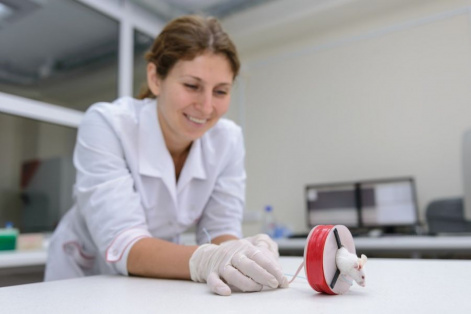
At that time, Krasnoyarsk media and Russian news agencies presented this work. Indeed, from some enthusiastic reports it was possible to understand that scientists were about to start treating people for cancer using gold nanoparticles. But so far, only experimental animals have been able to achieve consistent results. For further use of the method in medicine, it is necessary to carry out full preclinical and clinical trials of the drug.
Therefore, experiments in scientific laboratories continue. New publications are being prepared, and there appear interesting, sometimes unexpected results.
The journalist of the digital news edition "Our Krasnoyarsk Region" talked about this with one of the members of the team working on the project.
From the life of bioconjugates
Today, the guest of the “Territory of New Ideas” is Sergey Vasilievich Karpov, a specialist in the field of optics and nanostructured materials, Doctor of Physical and Mathematical Sciences, Professor of the Institute of Engineering Physics and Radioelectronics of the Siberian Federal University and International Research Center for Spectroscopy and Quantum Chemistry of the Siberian Federal University, Leading Researcher of the Laboratory of Coherent Optics at the Institute of Physics named after LV Kirenskiy SB RAS, Head of the Department of Physics, Siberian State University. M.F. Reshetnev. Sergey Karpov devoted 40 years of his life to science, he is the author of almost two hundred articles and monographs.
- Sergey Vasilyevich, for a humanitarian ear it sounds a little scary: nanoparticles, aptamers, DNA molecules, bioconjugates ... Could you tell in simple terms what this method of influencing cancer cells is? And how did you, a physicist, an optician, get into a project related to medicine?
- The use of a laser, including in medicine, is one of the areas in which we are engaged in the laboratory of coherent optics.
Several years ago I was approached by scientists from the Krasnoyarsk Medical University, Tatyana Nikolaevna and Sergey Sergeevich Zamay. They deal with the effects of various physical factors on malignant neoplasms. Their daughter, Anna Kichkailo, being in charge of the laboratory of digital controlled drugs and theranostics of the Federal Research Center of KSC SB RAS, is also engaged in this topic.
They asked me to participate in experiments using our resources and developments.
That's how we, physicists and doctors, started working together. In general, this topic is already known in the world, but we were faced with the task of simulating specific situations using well-known methods.
To put it briefly, a solution of gold nanoparticles is injected with a syringe into the blood of an experimental animal. Their size varies from 10 to 100 nanometers. This is about several tens of thousands of atoms.
It is very important that each of these particles is “coated" with DNA aptamers - these are molecules or DNA fragments that have the ability to selectively precipitate on cancer cells, or “to bind” to them. For this they have a key-lock recognition system.
So, owing to aptamers, nanoparticles "cling" to diseased cells, bypassing healthy ones.
We then introduce a fiberoptic waveguide into the tumor. The diameter of the waveguide can vary from one to several millimeters. Thus, laser radiation is transmitted, pulsed or continuous, acting on nanoparticles absorbing light. The so-called surface plasmon resonance is excited in the nanoparticle: electrons begin to oscillate relative to the crystal lattice with the frequency of the external field. They swing and heat the particle itself in tens of picoseconds. The particle, in turn, heats the liquid around itself…And thus, there occurs the transfer of thermal energy to the membrane of the diseased cell. This cell overheats and dies while healthy cells remain intact. This method is called hyperthermia.
- And what was your task here as a physicist?
- We build models and try to understand what impact is required in each specific case: continuous radiation or pulsed? What should be its duration and intensity?
Doctors are to deal with different types of oncological neoplasms, and, of course, for each of them different impacts are needed. What I am doing in the project as a physicist is called photonics or nanophotonics. This is a branch of optics which studies the interaction of light with very small fragments of matter, nanoparticles.
Note that the maximum absorption of light by spherical nanoparticles lies in the visible spectral range: approximately from 400 to 700 nanometers. For the human body, this is not the optimum range, because the strongest absorbent of optical radiation is our blood, which contains hemoglobin.
This means that it is necessary to use the radiation for which the blood is transparent and does not create obstacles. And this is precisely the range of 700-800, which has longer wavelengths. Here, we suggested using particles which consist of a core and a golden shell.
The core is made of zinc oxides with a certain fraction of aluminum atoms. The golden shell is extremely necessary, because only aptamers attach to gold. Such two-component nanoparticles make it possible to use laser radiation more efficiently.
- There is another way we are now working on. It is described in articles to be published soon. Your newspaper is the first I tell about this.
This method involves nanobubbles. Here, pulsed laser radiation and the same scheme is used: particles are localized on the membrane of a malignant cell. We increase the radiation intensity, and a vapor shell appears around the particles. That is, they heat up so much that the liquid medium of blood, so to say, the water boils. At the moment of the formation of this vapor shell there occurs a strong increase in pressure in front of its front, and a quasi-shock wave is created, which propagates in the liquid. Its strength is an order of magnitude higher than the strength of the cancer cell membrane. The membrane gets damaged. And since there are a lot of such nanoparticles on the membrane, they “collectively” destroy it, and the diseased cell dies.
- As I see, experiments are going on around “what other bullying a cancer cell can be subjected to”?
- We tried to "affect" it by a magnetic field. So, we took nanoparticles, in which the magnetite core is one of the iron oxides. While gold does not interact with a magnetic field, such particles does it very efficiently, because they are essentially microscopic magnets.
An animal inoculated with a complex carcinoma and injected with such nanoparticles was placed in an alternating magnetic field. Thus, unique results were obtained. Almost occasionally, one might say. The carcinoma is gone! The team of Professor T.N. Zamay published an article about this.
All the three methods: hyperthermia, vapor nanobubbles and exposure to magnetic fields are the subject of thesis of one of our post-graduate students. This is what we, physicists, are doing in the interests of medicine. Such research is of enormous importance for the development of new methods of cancer treatment, and many leading scientific centers around the world are working on this subject.
- But let us remind the readers that all these methods have been tested so far on laboratory animals. And although the results are encouraging, people in Russia are not yet treated with this method, right?
- Unfortunately, not yet. The set of methods of physical impact on a malignant cell is still in the process of formation. I heard that in Germany they are already trying to introduce this into medical practice. We still have a lot of work ahead of us, both in laboratories and clinics.
Source: Our Krasnoyarsk Region
Share:
